Top factors that inflate your corporate health insurance quote
See what drives up corporate health insurance premiums and what HR teams can do about it
By Pazcare
January 28, 2026

Total estimated yearly premium
*only basic terms and conditions applied
₹ 100,000
₹ 5,000 per life
Talk to our experts to get exact premium estimates
Schedule Call NowOur insurance advisors are looking into it. You can expect a call back in the next 10 minutes.
OkayGroup Health Insurance Claim Forms
The MDIndia reimbursement claim form for a group health insurance plan contains two parts. MDIndia claim form part A, which is duly filled by the policyholder or the primary insured. The second part is the MDIndia claim form part B, which is filled by the non-network hospital where the treatment was taken.
Download the MD India Claim form
Also read: Health insurance claim process
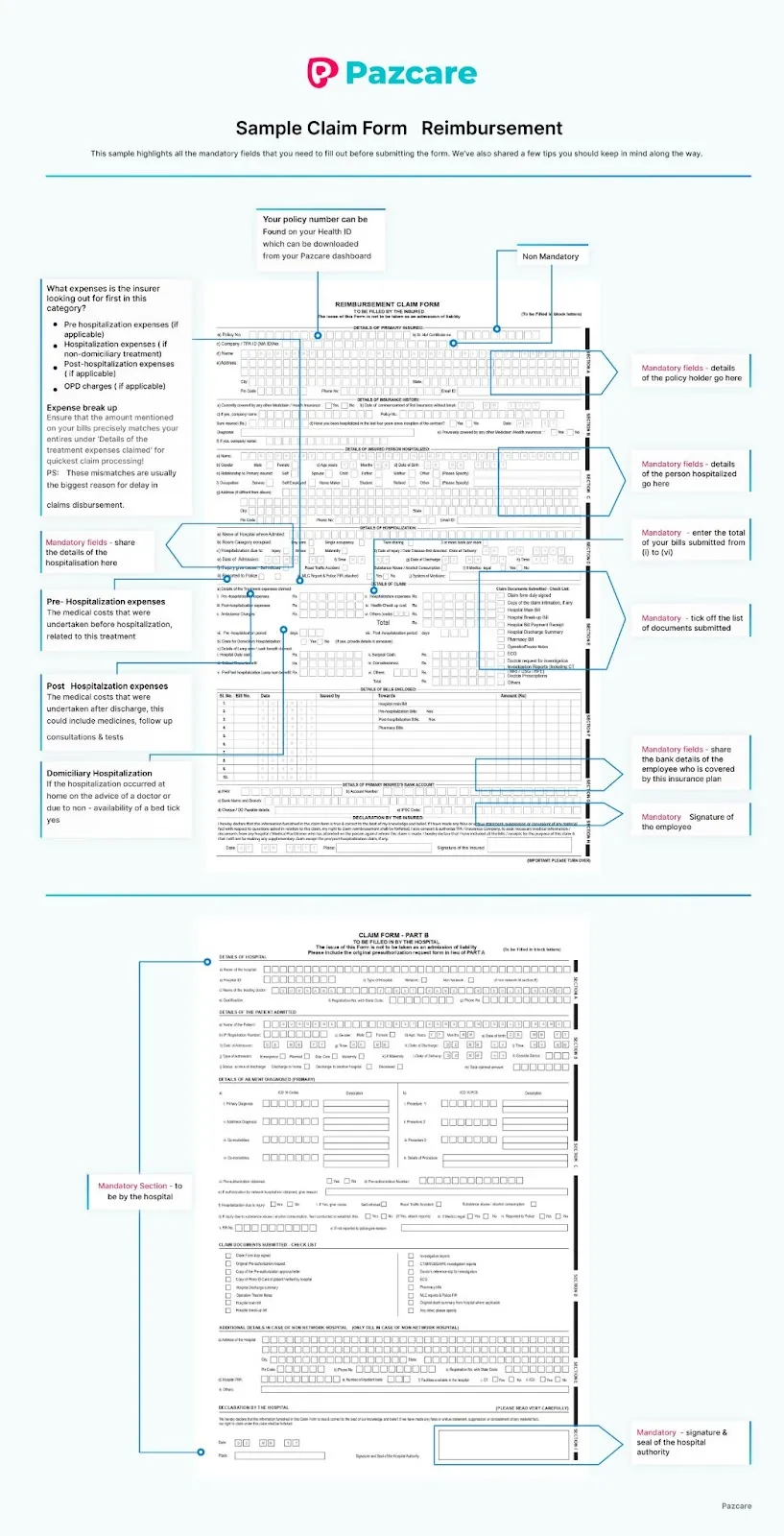
After you fill out the MDIndia claim form, here is how you will file for the reimbursement claim.
Download the MD India Claim form
Rating based on
4.6 / 5
Rating based on
(3023 reviews)
4.4 / 5
Rating based on
(2193 reviews)
4.8 / 5
Rating based on
(913 reviews)
4.2 / 5
Rating based on
(1267 reviews)
MDIndia Claim Form group health insurance customer care number
For any queries or assistance, reach out to us at any time. We provide 24X7 customer assistance.
Pazcare
Available 24X7
The MDIndia TPA customer care toll-free numbers are 1800 209 77 77, 1800 209 78 00, and 020 25300 126
24X7 customer assistance for queries, assistance and claim support
Looking for the best group health insurance for your team?
Have questions? We are here to help
© 2022 Insurance products are offered by Get Paz Insurance Brokers Pvt Ltd IRDAI Broking License Registration Code: Certificate No. 780, License category- Direct Broker (Life & General), valid till 17-Nov-2027.
Best pricing for you.
Best claim support for your team.

AICPA SOC 2
.svg)
ISO 27001
.svg)
ISNP